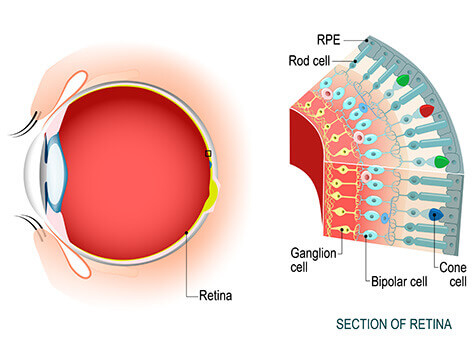
Retina is the thin inside lining of the eyeball. It acts like a film in the camera to capture the images. There are many diseases of the retina. Common ones are macular degeneration, diabetic retinopathy, floaters and flashes, retinal detachment, ocular migraine, epiretinal membrane, macular hole, and other less common conditions.
Lee Eye Center provides complete eye examinations including a retinal examination to detect and treat these conditions. People over the age of sixty need to have periodic retinal examinations once every 1-2 years.
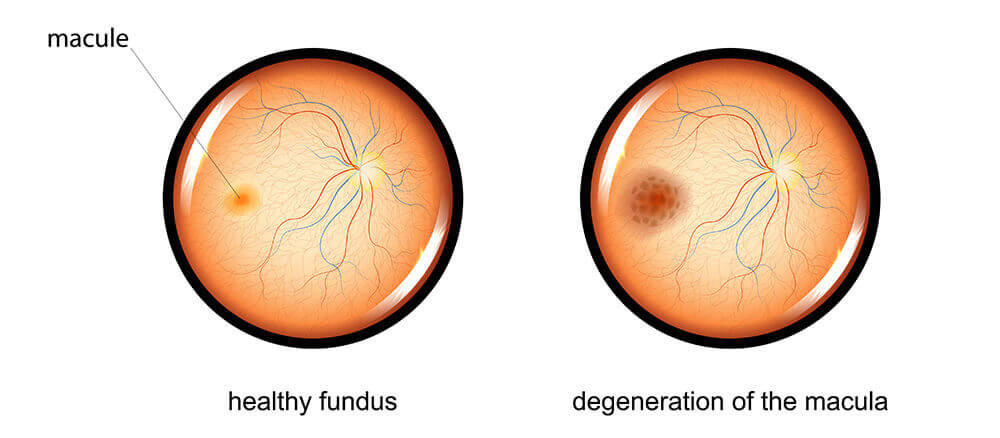

AMD is a serious disease that may result in loss of central vision. The exact cause is not known. It occurs when there is damage to the macula, the part of the eye that allows you to see fine detail. AMD does not affect peripheral, or side vision. Although people rarely go totally blind from the disease, AMD can make it difficult to read, write, drive or perform other normal daily tasks.
There are two kinds of AMD:”dry” and”wet”. Dry AMD affects about 90 percent of patients with AMD. It usually develops slowly, so people may not notice any change in their vision right away. Both eyes may or not be affected. A common early sign of dry AMD is the formation of yellow deposits, called drusen, under the macula.
Dry AMD can sometimes turn into wet AMD. Wet AMD affects only 10 percent of AMD patients, but it is responsible for 90 percent of all severe vision loss from the disease. Wet AMD occurs when abnormal blood vessels develop and leak blood and fluid under the macula, causing damage that leads to rapid loss of central vision.
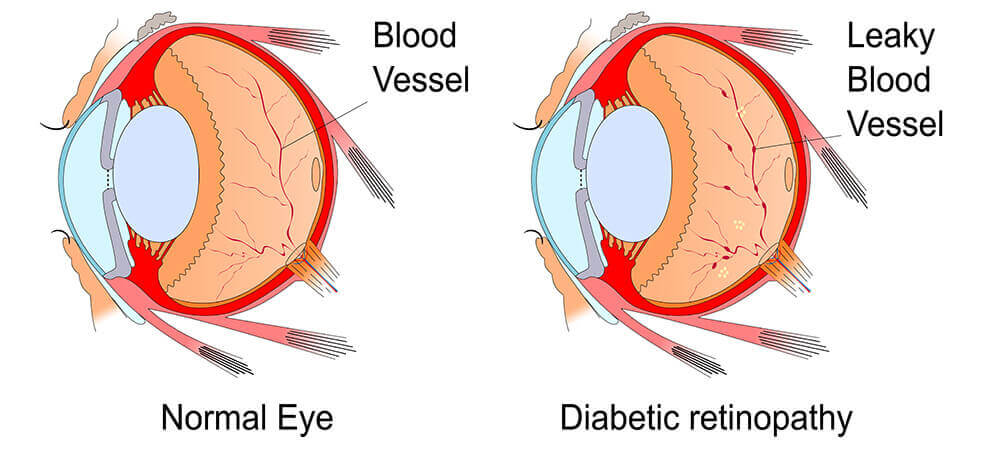
If you have diabetes mellitus, your body does not use and store sugar properly. High blood-sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy. It is critical that people with diabetes have an annual complete eye examination even if they do not have vision symptoms and show no signs of retinal damage on previous eye examination.
There are two types of diabetic retinopathy: non-proliferative diabetic retinopathy (NPDR) and proliferate diabetic retinopathy (PDR).

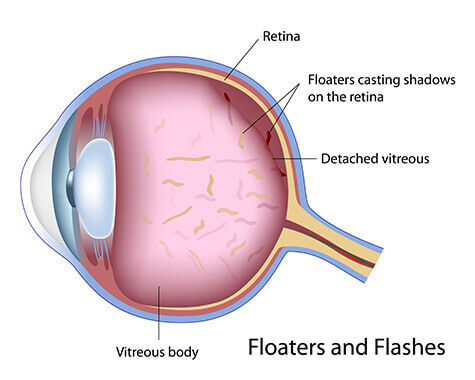
You may sometimes see small specks or clouds moving in your field of vision. These are called floaters. You can often see them when looking at a plain background, like a blank wall or blue sky. Floaters are actually tiny clumps of cells or material inside the vitreous, the clear gel-like fluid that fills the inside of your eye.
While these objects look like they are in front of your eye, they are actually floating inside it. What you see are the shadows they cast on the retina, the layer of cells lining the back of the eye that senses light and allows you to see. Floaters can appear as different shapes, such as little dots, circles, lines, clouds or cobwebs. As we grow older, it is more common to experience floaters and flashes as the vitreous gel changes with age, gradually pulling away from the inside surface of the eye.
When the vitreous gel pulls on the retina, you may see what look like flashing lights or lightning streaks. These are called flashes. You may have experienced this same sensation if you have ever been hit in the eye and seen “stars.” The flashes of light can appear off and on for several weeks or months. Flashes can sometimes lead to a tear in the retina. A retinal tear frequently needs to be treated with a laser. Left untreated, a retinal tear allows fluid to track behind the retina, separating it from the wall of the eye called a retinal detachment, which is a vision-threatening condition. So, new flashes and floaters require an urgent call to your eye doctor for a thorough retinal examination.
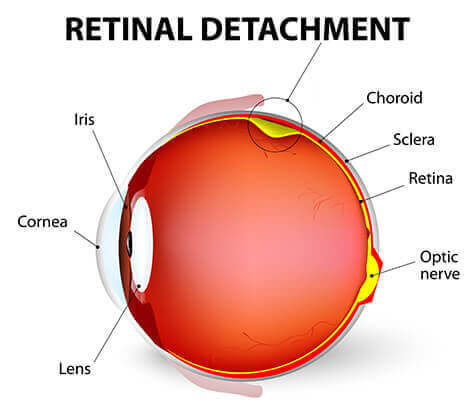
Retinal detachment is a separation of the retina from its connection at the back of the eye. The separation usually results from a tear (that is, a rent or rip) in the retina, which often occurs when the vitreous gel pulls loose or separates from its attachment to the retina. Once the retina has torn, the vitreous liquid can pass through the tear and accumulate behind the retina. The build-up of fluid behind the retina is what separates (detaches) the retina from the back of the eye. Vision loss occurs if the detached retina is not repaired. Early detection and treatment of retinal detachment are critical to prevent significant long-term vision loss.
Treatment options depend on the location and size of the retinal detachment. A small retinal detachment can be treated with laser alone, or in-office gas bubble, or both. A larger retinal detachment requires surgery to reattach the retina along with laser treatment and gas bubble. Sometimes an elastic band around the eye called scleral buckle is necessary. The gas bubble gets absorbed over several weeks. Until the gas bubble disappears, flying must be avoided to prevent gas expansion at high elevation that can cause eye damage from increased eye pressure.
Ocular migraine (also known as retinal migraine, ophthalmic migraine, optic migraine, visual migraine) is a painless, temporary visual disturbance that can affect one or both eyes. Though they can be frightening, ocular migraines typically are harmless and self-resolve without medication within 10 to 30 minutes.



It appears migraines are triggered by activation of a mechanism deep in the brain, which releases inflammatory substances around the nerves and blood vessels of the head and brain. Common external triggers for susceptible individuals include certain foods, such as caffeinated drinks, chocolate, nuts, aged cheese, smoked meats, MSG, artificial sweeteners, cigarette smoke, perfumes, lack of sleep and emotional stress.
The vision disturbances that occur with migraines usually go away after the migraine attack passes. Some migraine sufferers find that resting during an attack helps. If the trigger can be identified, just avoiding it will reduce frequency of the attack. As always, let your doctor know about your symptoms to make sure they are caused by a migraine and not a more serious issue, like a retinal tear or detachment.
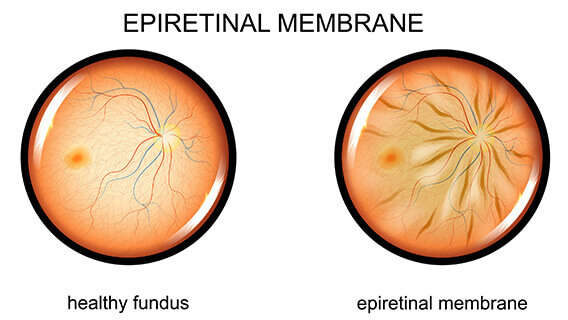
Epiretinal membrane (also known as macular pucker, cellophane maculopathy, pre-macular fibrosis) is the formation of a thin, fibrotic membrane over the retina, particularly the macula (the part of the eye responsible for detailed, central vision) that contracts, wrinkling the underlying retina and interfering with vision.

Sometimes when the vitreous pulls away from the retina, there is microscopic damage to the retina’s surface (Note: This is not a macular hole). When this happens, the retina begins a healing process to the damaged area and forms scar tissue, or an epiretinal membrane, on the surface of the retina. This scar tissue is firmly attached to the retinal surface. When the scar tissue contracts, it causes the retina to wrinkle, or pucker, usually without any effect on central vision. However, if the scar tissue has formed over the macula, our sharp, central vision becomes blurred and distorted.
For most people, vision remains stable and does not get progressively worse. Usually, the epiretinal membrane affects one eye, although it may affect the other eye later.
An epiretinal membrane usually requires no treatment. In many cases, the symptoms of vision distortion and blurriness are mild, and no treatment is necessary. People usually adjust to the mild visual distortion, since it does not affect activities of daily life, such as reading and driving. Neither eye drops, medications, nor nutritional supplements will improve vision distorted from epiretinal membrane. Sometimes the scar tissue (which causes a macular pucker) separates from the retina, and the macular pucker clears up.
Rarely, vision deteriorates to the point where it affects daily routine activities. However, when this happens, surgery may be recommended. This procedure is called a vitrectomy, in which the vitreous gel is removed to prevent it from pulling on the retina and replaced with a salt solution. Since the vitreous is mostly water, you will notice no change between the salt solution and the normal vitreous. Also, the scar tissue which causes the wrinkling is removed. This special vitrectomy along with removal of scar tissue is also referred to as a membrane peel. It is usually performed under local anesthesia. After the operation, the patient needs to wear an eye patch for a few days or weeks to protect the eye and also needs to use medicated eye drops to protect against infection and speed up healing.
Macular hole is a small, circular break in the macula.
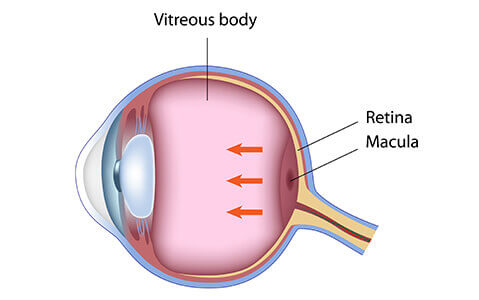
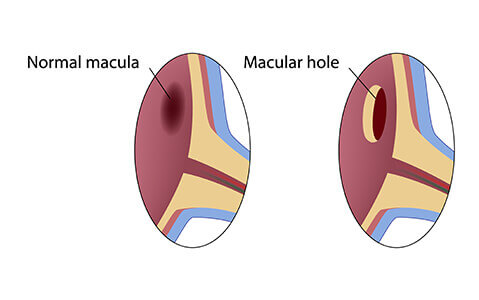
Shrinking of the vitreous, a jelly-like substance in the back of the eye, usually is the cause of a macular hole. As a person ages, the vitreous becomes watery and begins to pull away from the retina. If the vitreous is firmly attached to the retina when it pulls away, a hole can result.
Macular holes often begin gradually but can be sudden. In the early stage of a macular hole, people may notice a slight distortion or blurriness in their straight-ahead vision. Straight lines or objects can begin to look bent or wavy. Reading and performing other routine tasks with the affected eye become difficult.
Although some macular holes can seal themselves and require no treatment, surgery is necessary in many cases to help improve vision. In this surgical procedure, called a vitrectomy, the vitreous gel is removed to prevent it from pulling on the retina and replaced with a bubble containing a mixture of air and gas. A thin membrane over the macula is also removed to allow the cells to migrate in to seal the hole. The bubble acts as an internal, temporary bandage that holds the edge of the macular hole in place as it heals. Surgery is performed under local anesthesia and often on an out-patient basis.
Following surgery, patients must remain in a face-down position, normally for a day or two but sometimes for as long as two-to-three weeks. This position allows the bubble to press against the macula and be gradually reabsorbed by the eye, sealing the hole. As the bubble is reabsorbed, the vitreous cavity refills with natural eye fluids. Maintaining a face-down position is crucial to the success of the surgery. Because this position can be difficult for many people, it is important to discuss this with your doctor before surgery.